Live
Support AI
Limb Lengthening Post-op Period, Problems And Complications
Limb lengthening surgery has become increasingly popular in recent years. Some patients opt for this surgery due to health issues (like dwarfism or having one shorter leg), while others choose it purely for aesthetic reasons, aiming to look taller and more attractive. It's important to note that limb lengthening is a long and challenging process, and it's crucial for patients to be well-informed about the surgery.
In the continuation of our article, we will be sharing details about the post-surgery process and providing information about the techniques used in the surgery. If you wish to learn more about the methods, you can check the limb lengthening surgery methods on our website.
Early Post-Operative Period After Limb Lengthening Surgery (Latent Phase)
After the limb lengthening surgery, nurses teach patients how to clean the areas around the pins, which connect the external device to the leg. This "pin care" is crucial and takes about 30-40 minutes daily. It helps prevent infections. Patients learn to spot early signs of infection, like warmth, swelling, and redness. If a pin area gets red and painful, especially with unusual discharge, they might need antibiotics.
Distraction Phase
 Once the initial recovery period (roughly 7-10 days post-surgery) is over, the process of bone lengthening begins. By this point, you'll know how to operate the device correctly. The bone typically extends by about 0.5 – 1 mm daily. This rate can be adjusted faster or slower based on your doctor's recommendations and how things are progressing.
Once the initial recovery period (roughly 7-10 days post-surgery) is over, the process of bone lengthening begins. By this point, you'll know how to operate the device correctly. The bone typically extends by about 0.5 – 1 mm daily. This rate can be adjusted faster or slower based on your doctor's recommendations and how things are progressing.
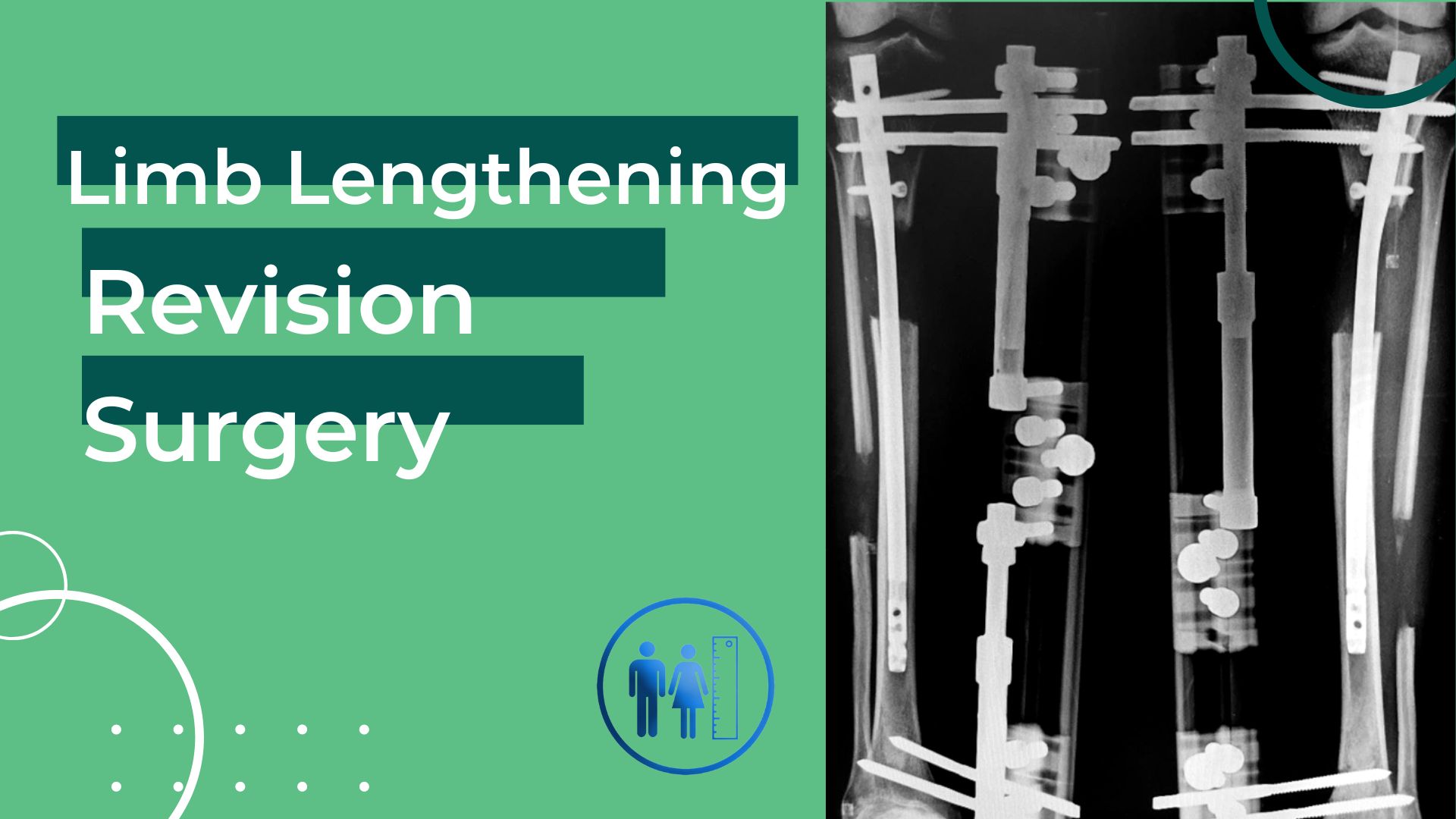
Most complications from the treatment arise during the distraction phase, so the surgeon needs to be cautious for any known issues. During this phase, patients should have check-ups at least every two weeks. These appointments should include a thorough clinical review and X-ray examinations. Out of town patients can just send X-rays and physical therapy reports instead of coming in.
After reviewing the x-rays, the doctor email patient, or patient has an online consultation with the doctor, where he/she is given updated weight-bearing instructions depending on the progress of the consolidation (if patient has a surgery with intramedullary nailing system) and other problems or concerns one may have, also is discussed. Specifically, the doctor measures the length of distraction and assesses the degree of maturity of the “regenerate” (the newly formed bone in the area of distraction).
Consolidation Phase
When the lengthening of the bone to the planned length has been completed, the newly formed callus (it is also called “Regenerate”) needs time to strengthen and to convert to normal bone with satisfactory weight bearing ability. This phase is called consolidation.
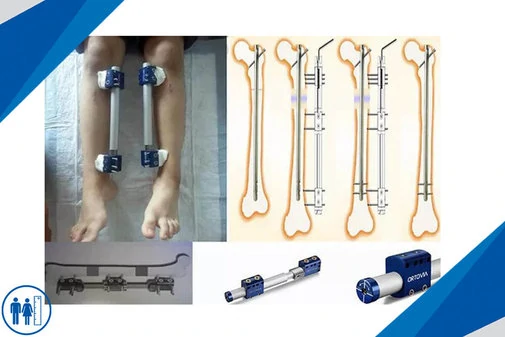
The fixator will remain until the end of the consolidation phase to allow the newly-formed bone to harden. No further adjustments are made to the fixator. For patients who had surgery with Ilizarov method or other external fixators, the device is removed when new bones are able to carry patient’s weight.
Before removing the frame, a 'stress test' may be given to the patient. In this test, all connections between the upper and lower bone segments are detached, and the patient is asked to use the limb normally (like bearing weight for the lower limb or carrying out tasks for the upper limb). If the patient manages this successfully, the frame can be confidently taken off. While the removal process typically happens under anesthesia because taking out the half pins can be quite painful.
During the consolidation phase, if you have a Precice Nail, you will continue to walk with weight bearing restrictions. No more alterations will be made to the PRECICE nail. The PRECICE nail will remain in place throughout the consolidation phase to support the regenerate bone. Depending on the bone that has been lengthened, the length of the regenerate and individual parameters of the patient, full weight bearing is usually allowed between 6 and 8 weeks after the end of the lengthening phase.

The implantable lengthening device is constructed from non-reactive metals, specifically either titanium or stainless steel. The specific timing for the removal of the device is not highly time-sensitive, and it is advised to be carried out within a timeframe of 1 to 2 years after its initial insertion. The process of removing the device can be performed on an outpatient basis. Removing implanted metal devices necessitates another surgical procedure that is conducted while the patient is under general anesthesia.
During the consolidation phase, the risk of complications decreases significantly, and the patient's functional abilities improve. Encouraging movement and ambulation is essential to promote a swift consolidation of the newly formed bone. Several factors, including the patient's age, the bone segment involved (femur or tibia), the location of the corticotomy, and the size of the osteotomy gap, have a substantial impact on the bone-healing process. It's worth noting that the time required for distraction and consolidation relative to the size of the distraction gap is notably shorter for femoral lengthening compared to tibial lengthening. Patients aged 20 and older tend to experience slower healing than those younger than 20. Additionally, patients aged 20 to 29 generally heal more quickly than individuals older than 30 but at a slower rate than those under 20 years old.
Lengthening over Nail (LON Method)
A different strategy for the distraction and consolidation phases aims at reducing the total fixator time by simultaneously placing an intramedullary solid nail at the time of osteotomy and by removing the external device at the end of distraction. After the distraction phase, the nail is locked to stabilise the gained length and axis before removal of the fixator.
Physiotherapy
When it comes to limb lengthening surgery, we can undoubtedly say that physiotherapy is one of the most crucial and critical aspects of this process. After the surgery, in order for the patient to recover quickly and healthily, physiotherapy should be applied consistently, and especially wound care around the surgical site should be done regularly. Patients who neglect their physiotherapy sessions will experience muscle weakness, which can have highly unfavorable consequences when it comes to returning to their daily activities.
Therefore, if you are considering limb lengthening surgery, you should not perceive this process as just having a surgery and then immediately returning to your daily life. You should conduct your research with the understanding that the healing process is long and challenging, and it is essential to always coordinate with your doctor.
Complications and risks
As with any surgery, it is possible for some complications to occur after limb lengthening surgery, although it is not very common in cases where treatments are carried out correctly. Nevertheless, it is crucial for patients planning to undergo surgery to have knowledge about potential complications during this process.
Post-operative complications are primarily related to hygiene and physiotherapy. To explain this with a few examples, it can be said that, first and foremost, patients should stay in communication with their doctors throughout the treatment period. They should follow their doctors' instructions for wound care, wound cleaning, and physiotherapy sessions.
Patients who do not adhere to doctor's instructions, such as not regularly attending wound dressing appointments, increase the likelihood of permanent scarring. Similarly, insufficient disinfection of the surgical site can lead to infections in that area, resulting in leg pains and, in some cases, more serious problems. Another possible scenario is not attending physiotherapy sessions as recommended by your doctor. Disrupting your treatment can weaken your leg muscles, thus negatively affecting the healing process. As a result, returning to your daily life will take much longer. Complications like these can occur due to interruptions in your treatment process. Therefore, it is essential to pay attention to your doctor's guidance and take the necessary care during this process.
Recovery Period
During the recovery period, physical therapy plays a very important role in keeping the patient’s joints flexible and in maintaining muscle strength. Patients are advised to eat a nutritious diet (milk and milk products, sesame, Dark leafy greens, sardines and etc.) and to take calcium supplements. To speed up the bone healing process, gradual weight-bearing is encouraged. Open wounds and broken bones are also heal faster in sunlight. Without sunlight, the bones cannot become calcified. Patients are usually provided with an external system that stimulates bone growth at the site, either an ultrasound device or one that creates a painless electromagnetic field.
You will be informed about the lengthening increase, lengthening process, the prices of the surgical methods, the difference of the methods, the risks of the surgery.